Abstract
Introduction:
Multiple myeloma (MM) is the 14th leading cause of cancer deaths in the USA. According to NIH cancer statistics, there will be estimated 30,280 new cases and 12,590 deaths due to MM in 2017. Immunotherapy appears to be an appealing treatment modality for MM. Various immunotherapeutic approaches are being used and our aim is to summarize current knowledge on efficacy of non-FDA approved monoclonal antibodies (mAbs), chimeric antigen receptor modified (CAR-T) cells and their targets.
Methods:
For CAR-T cells literature search was performed on 7/16/2017 in following databases: PubMed, Cochrane, EMBASE, Web of Science and Clinicaltrilas.gov. Only English language studies were included and no publication date limit was applied. For mAbs, phase I/II trials that were complete or recruiting participants were retrieved from clinicaltrials.gov on 7/19/2017. Trials on elotuzumab and daratumumab that have already proven efficacy were not included.
Results:
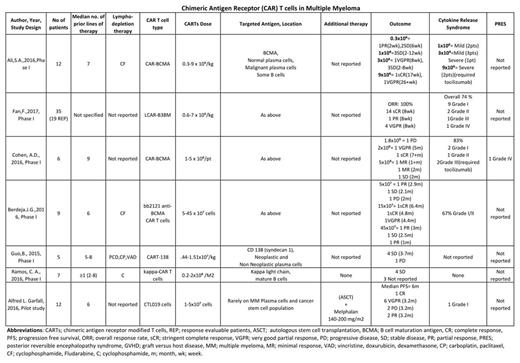
Literature search identified a total of 287 articles on CAR-T cells. After detailed scrutiny, 6 studies were included. Citation analysis retrieved one additional study. 7 studies included 86 relapsed and refractory MM (RRMM) patients. Targeted antigens included B-cell maturation antigen (BCMA) (n=4 studies), CD138 (n=1), CD19(n=1) and kappa light chain (n=1). There was significant variation in CAR T cell dose ranging from 1 x 10⁷ to 5 x 10⁸ per patient. Most patients were heavily pretreated with ≥ 6 median prior lines of therapy. Only one study additionally incorporated ASCT. No objective response (OR) was achieved with CD138 and kappa light chain directed CAR T cell therapy. For BCMA and CD19 directed CAR T cell therapy, there was significant variation in efficacy outcomes reported with PR ranging from 2 weeks to 3.2 months (m), VGPR 2m to 5m and sCR 2m to 7+m. Highest incidence of cytokine release syndrome (CRS) of all grades was reported with BCMA directed CAR T cell therapy, ranging from 58-83%. One case of posterior reversible encephalopathy syndrome was reported with BCMA targeted CAR T cell therapy.
mAb targets included ICAM-I (BI-505), IL-6 (siltuximab), VEGF (bevacizumab), GRP78 (PAT-SMX), CD40 (dacetuzumab, lucatumumab), CD138 (indatuximab), PD-1 (pembrolizumab, nivolumab, pidilizumab), CD20 (rituximab), CD38 (isatuximab), CD56 (lorvotuzumab), IGF-1R (AVE1642, figitumumab), VEGF (bevacizumab), BAFF (atacicept, tabalumumab) and CD74 (milatuzumab). No objective response (≥PR) was observed with monotherapy with BI-505, siltuximab, bevacizumab, PAT-SMX, AVE-1642, figitumumab, atacicept, milatuzumab, dacetuzumab and nivolumab. Isatuximab (anti-CD38) was the only mAb with promising results (OR 24%) as monotherapy in patients with 6 prior lines of therapy. Most trials employed RRMM patients. Siltuximab in combination with VMP (velcade, melphalan and prednisone) was evaluated in frontline setting without significant improvement reported (CR of 22% vs 27% with VMP alone and PFS of 17 months in both arms). Antibodies tested as conjugates include indatuximab, ravtansine (anti CD138) and lorvotuzumab mertansine (anti CD56). Their results were encouraging when used in combination with Rd (lenalidomide and dexamethasone), OR of 78% with indatuximab +Rd and 56.4% with lorvotuzumab +Rd. MAbs that've been tested in combination therapy include siltuximab (S+Vd, OR 66%), dacetuzumab (D+Rd, OR 39%), indatuximab (I+Rd, OR 78%), isatuximab (I+Rd, OR 64.5%), lorvotuzumab (L+Rd, OR 56.4%) and pembrolizumab (P+Pd, OR 50%).
Conclusion:
Immunotherapy with mAb and CAR-T therapy seems to offer very promising results. Short term and log term toxicity with mAb and cellular therapy demands thorough understanding of mechanism, biology behind the " on target" and "off target" effects, side effect profile and their prevention. Further trials are warranted to determine best CAR-T cell construct and design for treating MM. Outcomes with many single agent mAb therapy were not encouraging and provide a rationale that future trials with mAbs should be done as multi-agent therapies. Promising results with isatuximab warrants further trials. Antibody-drug conjugate treatment is worth further evaluation both as single agent and in combination with standard anti-MM agents. Individualized treatment approach based on surface CD marker expression need to be developed and may produce better outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal